Research
Insulin Overdose: Signs, Treatment, and Prevention
If you’re asking yourself “can you overdose on insulin?,” you should know this is a real possibility. Here’s the US MED guide to handling an insulin overdose.
Read MoreCan You Trust Your Diabetic Supply Company? 3 Signs to Look For
You depend on your diabetic supply company to provide you with safe, quality supplies for managing diabetes. How do you know if your Durable Medical Equipment (DME) provider is legitimate? Are you receiving genuine name brand products or knockoffs? Read on to learn about 3 signs to look for when choosing the safest and most…
Read MoreManaging Diabetes and Depression: Strategies for Your Mental Health
Both diabetes and depression can be difficult conditions to manage – and that’s especially true when you’re dealing with both at the same time. Get advice on how to cope from US MED.
Read MoreCan Stress Raise Blood Sugar? | A Guide to Managing Stress and Diabetes
If you suspect stress may be affecting your ability to manage your diabetes, you’re not alone. Medical professionals have looked into possible connections between stress and diabetes since the 17th century. Today, scientific research indicates there may very well be a direct link between these two issues. Anyone who’s wondered “can stress and anxiety cause…
Read MoreThe Link Between Diabetes and Cardiovascular Disease: What You Need to Know
Maintaining optimal cardiovascular health is paramount for individuals navigating life with diabetes. It’s a reality that those managing diabetes face an increased likelihood of developing cardiovascular diseases (CVD), such as heart disease and stroke. In fact, CVD accounts for a significant portion of mortality among individuals with type 2 diabetes, comprising two-thirds of all deaths…
Read MoreThe Future of Diabetes Management: Why CGM and GLP-1s are a Symbiotic Pair
As a leader in the diabetes supplies industry, I have a front-row seat to the evolving landscape of care. One prominent discussion centers on the rise of GLP-1 semaglutide for type 2 diabetes. While some may see this as a threat to continuous glucose monitoring (CGM) technology, I believe the opposite is true: GLP-1s and CGM…
Read MoreThe Role of Technology in Diabetes Management: From Apps to Continuous Glucose Monitors
Since its discovery in 1921, insulin has played a central role in treating type 1 (and, in some cases, type 2) diabetes. But while this was undoubtedly a milestone in the history of diabetes management, technological progress hasn’t stopped there. Much more recent developments have also led to notable improvements in the lives of people…
Read MoreShoes, Diabetes, and Foot Health
Foot problems are common in people with diabetes, and wearing the right shoes is a great way to keep your feet safe. Learn more with US MED.
Read MoreMushrooms and Diabetes: How Can Mushrooms Help with Blood Sugar Levels?
Learn more with US MED’s guide to adding mushrooms to your diabetes diet and discover how this food can help keep your blood sugar in check.
Read MoreHow Does Diabetes Affect Sleep?
Are you wondering “how does diabetes affect your sleep?”. This is US MED’s overview of how sleep and diabetes type 2/type 1 intersect.
Read MoreWhat Body Shape Says About Health | Diet & Fitness
Learn all about different body shapes and what each shape might reveal about your health and well-being.
Read MoreDexcom G7 Release Date, Features & Cost Insights
Are you interested in learning more about the Dexcom G7 and what distinguishes it from other CGMs available today? If so, you’re in luck. Take a look at our complete overview of this exciting new product!
Read MoreKnow Your Diabetes ABCs | US MED
Learning essential diabetes management steps can make managing this disease far simpler. Learn the ABCs of diabetes with US MED.
Read MoreDoes Diabetes Cause High Blood Pressure?: Understanding Between High Blood Pressure and Diabetes
If you’re wondering, “can diabetes cause high blood pressure?” or “how can I control high blood pressure with diabetes?,” read on for all the answers you need.
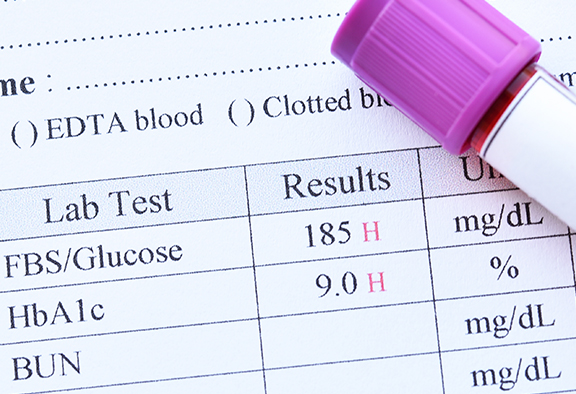
Read MoreA1C Overview: What is A1C? | US MED
One reliable method of diagnosing diabetes is the hemoglobin A1C test. If you’re asking yourself, “What is A1C testing, anyway?” Learn more with US MED.
Read MoreDiabetes Symptoms: What You Need to Know
Diabetes management isn’t always an easy task, but you’ll need to work hard at it. Learn about diabetes symptoms and management with US MED.
Read MoreDiabetes Rash: Appearance & Prevention
Diabetes can lead to complications in other areas, one of these being your skin. Learn more about what skin complications to be on the lookout for.
Read MoreHow to Choose a Glucose Meter
Need to buy a new blood glucose meter? It’s essential to make sure you’re getting a glucometer that’s a good fit for your needs. Read on for frequently asked questions, simple instructions, and a brand analysis.
Read MoreBuilding a Diabetes Care Plan
There’s a lot that goes into managing diabetes, including everyday personal care, lab tests, and going to the doctor. Use our template to stay on track to manage your diabetes.
Read MoreFlu and Diabetes: Symptoms and Treatment
The flu can lead to complications for people with diabetes. Learn why flu shots are recommended for use by people with diabetes.
Read MoreWhere to Inject Insulin & How to Keep Insulin Injection Sites Healthy
Studies have shown that almost two-thirds of all people who inject insulin have some degree of lipohypertrophy – thickening or rubbery skin at injection sites. Here, we discuss ways to avoid lipo and things to look out for.
Read MoreGestational Diabetes 101
Learn all about gestational diabetes and how it could affect your pregnancy.
Read MoreType 2 Diabetes | Overview, Symptoms, Causes, Treatment
Type 2 diabetes is a metabolic disorder that affects blood sugar levels in your body. Learn more about type 2 diabetes symptoms, causes, risk factors, and prevention.
Read MoreDiabetes Management | Living With Diabetes
Are you living with diabetes? We’ll walk you through some healthy lifestyle and routine choices that can help you better manage diabetes.
Read MoreImproving Circulation After DVT | DVT Recovery & Treatment
Help avoid a DVT and improve circulation in your legs. Learn all about how to reduce your risk of developing deep vein thrombosis.
Read More7 Unknown Advantages of The Diabetes Diet
Managing diabetes means caring about your whole-body health. Following the Diabetes Diet will help lower blood sugar, but it also does so much more. From weight loss to cancer prevention this diet helps from head to toe!
Read MoreIs There a Cure For Type 1 Diabetes
Read on to learn all about cutting-edge efforts to cure diabetes – and how you can stay healthy in the meantime.
Read MoreMore Than Two Types of Diabetes?
For the past 20 years diabetes has always been classified as either type 1 or type 2, but new revelations show that there could actually be five different types. New research such as one found in an article out of The Lancet: Diabetes & Endocrinology suggests a need for a revision to the diabetes classification system. …
Read MoreIdentifying Alzheimer’s before symptoms
New tests to diagnose Alzheimer’s disease are emerging, offering hope for new treatments and therapies. According to the Alzheimer’s Association, the memory disease is now the sixth leading cause of death in the United States, and more than 5 million people are currently living with the disease. In fact, for seniors, a third of all…
Read MoreThe Medical Supplies Market is Expanding
Market Research Future Report According to Market Research Future, the global medical supplies market is growing exponentially and expected to reach $132 Billion by late 2022. The primary cause of this massive growth is the rising population of geriatrics as well as increase in patients with chronic diseases such as cardiovascular & diabetes. Leading this sales…
Read MoreArtificial Beta Cells that Release Insulin in Response to High Blood Sugar
A major hurdle in the patient-friendly treatment of Diabetes is the need for efficient on-demand control of blood glucose levels. Normal pancreatic cells do this naturally, so creating an insulin delivery system has been quite a challenge for researchers. Insulin pills end up destroyed in digestive enzymes and acids making it an unviable option. Pancreatic…
Read MoreNewsletter Sign Up
Get the latest articles, news and special offers delivered right to your inbox!
*By clicking the button above, I agree to signing up to US MED's newsletter emails and consent to receiving emails from US MED.