Diabetes
5 Steps for Managing Diabetes | Type 1 and Type 2
We’ll walk you through five steps to help you manage your diabetes so you can live a life you love. Written by: US MED Staff Clinically Reviewed by: Shirley DeLeon, RD, CDCES Managing diabetes isn’t always easy. The process of dealing with this condition comes with all sorts of inconvenient testing requirements and dietary changes –…
Read MorePrediabetes: Key Risk Factors and Effective Lifestyle Changes
If you’re at risk for type 2 diabetes, you may develop a condition known as “prediabetes” first. Here’s US MED’s guide to prediabetes management. Written by: US MED Staff Clinically Reviewed by: Shirley DeLeon, RD, CDCES Many people who get diagnosed with type 2 diabetes feel like this disease came out of nowhere. In reality, that…
Read MoreComparing the Best Insulin Pumps: Features, Pros, and Cons for Managing Diabetes
What is the Best Insulin Pump for Your Diabetic Needs? Diabetes is a serious condition, and more people than ever are dealing with this disease today. According to the CDC, the number of adults with diabetes has doubled in the past two decades. Everyone with type 1 diabetes (and more than a few people with…
Read MoreInsulin Pumps and CGMs: A Complete Guide for Diabetes Management
How much is a CGM? How is an insulin pump different than a CGM? Get answers to these question and more in this product breakdown.
Read MoreHow to Apply a CGM Sensor
It’s no secret that continuous glucose monitors (CGMs) are popular among people with diabetes these days. If you’re wondering, “how is CGM inserted?,” keep reading for a complete guide to CGM installation and more.
Read MoreType 1 Diabetes vs Type 2 Diabetes
What is the Difference Between Type 1 Diabetes and Type 2 Diabetes? If you’ve recently been diagnosed with diabetes, you’re probably searching for clear answers about the differences between Type 1 diabetes and Type 2 diabetes. We know it can feel overwhelming, so we’re here to help distinguish between these two forms of the condition.…
Read MoreDo I Need a CGM Prescription? Answers for People with Diabetes
These days, most people with diabetes have at least heard of continuous glucose monitors (CGMs). These devices allow you to test your glucose levels by simply applying a sensor, significantly lowering your reliance on finger prick tests in the process. Are you wondering, “Do I need a CGM prescription?” If so, you’re in the right…
Read MoreManaging Diabetes and Depression: Strategies for Your Mental Health
Both diabetes and depression can be difficult conditions to manage – and that’s especially true when you’re dealing with both at the same time. Get advice on how to cope from US MED.
Read MoreManaging Diabetes When You’re Sick: Essential Tips
Many aspects of everyday life are more difficult when you’re managing diabetes, and that includes taking care of other illnesses. While colds and the flu can be inconvenient for anyone, having diabetes can increase your odds of getting seriously sick. Meanwhile, these conditions put extra stress on your body, potentially increasing your blood sugar levels…
Read MoreCan Stress Raise Blood Sugar? | A Guide to Managing Stress and Diabetes
If you suspect stress may be affecting your ability to manage your diabetes, you’re not alone. Medical professionals have looked into possible connections between stress and diabetes since the 17th century. Today, scientific research indicates there may very well be a direct link between these two issues. Anyone who’s wondered “can stress and anxiety cause…
Read MoreThe Link Between Diabetes and Cardiovascular Disease: What You Need to Know
Maintaining optimal cardiovascular health is paramount for individuals navigating life with diabetes. It’s a reality that those managing diabetes face an increased likelihood of developing cardiovascular diseases (CVD), such as heart disease and stroke. In fact, CVD accounts for a significant portion of mortality among individuals with type 2 diabetes, comprising two-thirds of all deaths…
Read MoreHow to Care for Diabetes: A Guide for Families and Caregivers
Navigating the journey of diabetes care can be complex, but with the right knowledge and support, managing diabetes becomes more manageable. At US MED, we’re dedicated to empowering families and caregivers with essential insights on how to care for diabetes, especially for aging loved ones who face unique challenges with their condition. No matter who…
Read MoreThe Future of Diabetes Management: Why CGM and GLP-1s are a Symbiotic Pair
As a leader in the diabetes supplies industry, I have a front-row seat to the evolving landscape of care. One prominent discussion centers on the rise of GLP-1 semaglutide for type 2 diabetes. While some may see this as a threat to continuous glucose monitoring (CGM) technology, I believe the opposite is true: GLP-1s and CGM…
Read MoreBest Blood Glucose Meters for 2024 | A Curated Guide
For people with diabetes, blood glucose meters aren’t just helpful—these devices are an essential component of any worthwhile diabetes management strategy. Still, some glucometers are better than others, so we’re here to shine a light on the best glucose meters on the market. And since you’ll be using your meter so often, it’s wise to…
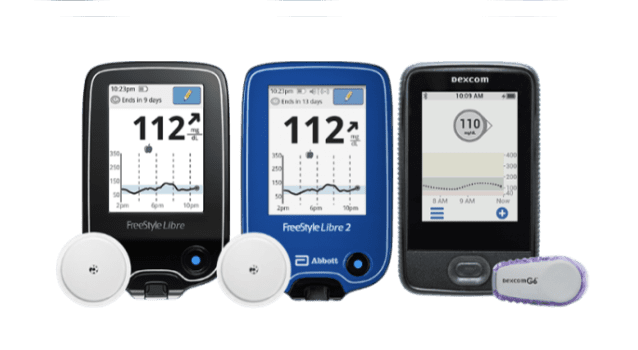
Read MoreDifferent Types of CGM: A Complete Guide
What is the Best Continuous Glucose Monitor (CGM) for Your Diabetic Needs? It’s a fact of life – people with diabetes need to check their glucose levels every so often. In the past, that meant doing multiple finger-prick tests per day. But these tests are inconvenient and painful, so it’s not hard to see why…
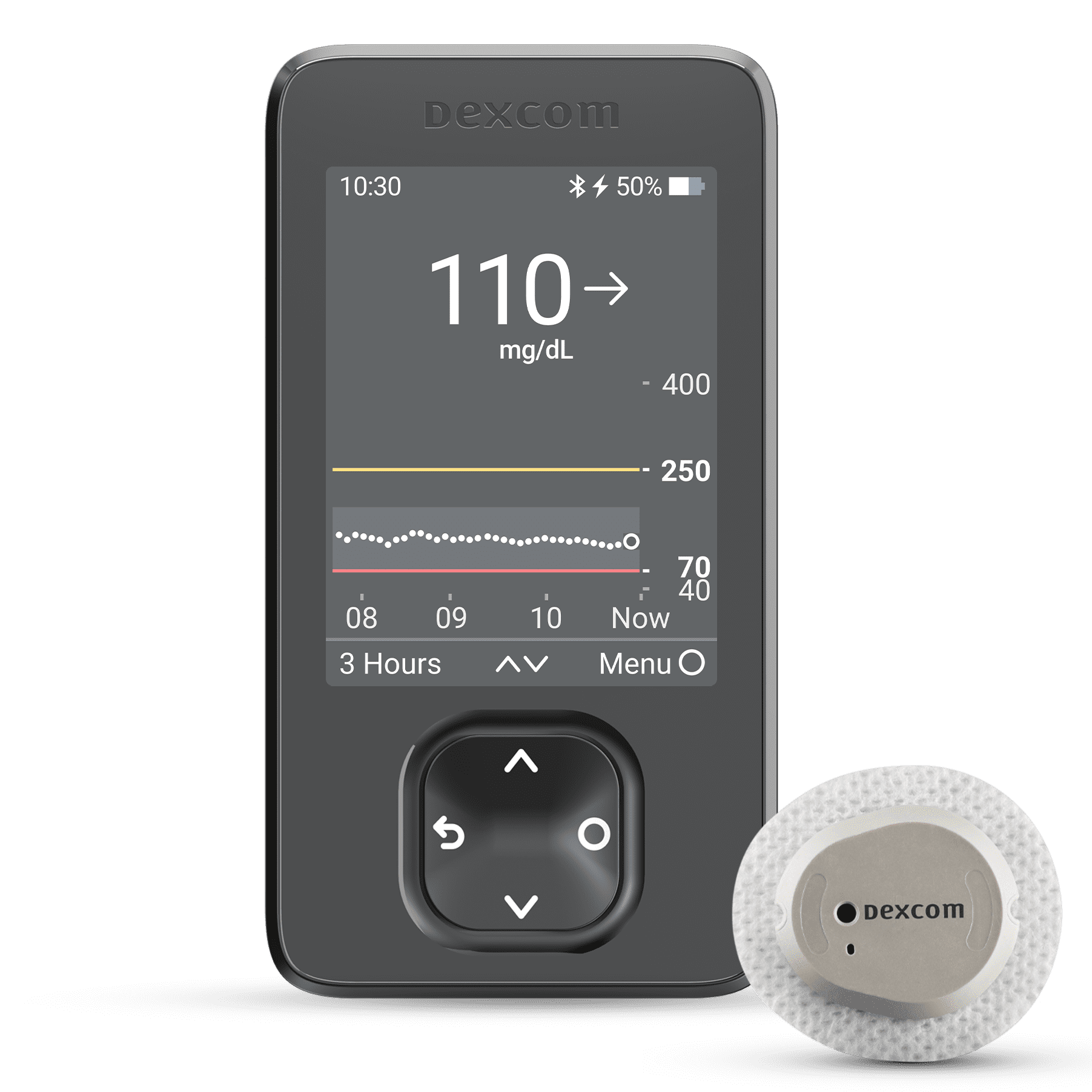
Read MoreDexcom G7 Compatibility with Tandem t:slim X2: What You Need to Know | US MED
In early 2023, Dexcom began offering the Dexcom G7 Continuous Glucose Monitoring (CGM) System to U.S. residents with diabetes. This system launched with features like unmatched accuracy*, a discreet and comfortable sensor†, and a warm-up time twice as fast as any other CGM‡. But when this device launched, it was missing one capability its predecessor…
Read MoreDiabetes and Dental Health: How to Protect Your Smile and Prevent Complications
Diabetes and Dental Health: How to Protect Your Smile and Prevent Complications Diabetes management can undoubtedly be stressful, but it’s best to face each day with a smile—though you’ll want to take a few steps to protect your smile first. In addition to diabetes complications such as heart problems and nerve damage, studies suggest a…
Read MoreThe Role of Technology in Diabetes Management: From Apps to Continuous Glucose Monitors
Since its discovery in 1921, insulin has played a central role in treating type 1 (and, in some cases, type 2) diabetes. But while this was undoubtedly a milestone in the history of diabetes management, technological progress hasn’t stopped there. Much more recent developments have also led to notable improvements in the lives of people…
Read MoreDiabetes and Family Support: Navigating the Impact and Outcome Together
Living with diabetes presents its challenges, and as a family member or caretaker, your support is crucial. Diabetes requires constant management and doesn’t just disappear over time. With approximately 28.7 million diagnosed cases in the US alone, it’s clear that many families are affected by this condition. Your loved one needs a strong support system…
Read MoreIntermittent Fasting and Diabetes: Potential Benefits and Consideration
In this article we take a closer look at Intermittent Fasting and share with you the risks and benefits.
Read MoreHaving a Social Life and Navigating Events with Diabetes
Managing diabetes can be difficult enough as it is. This is US MED’s guide on how to balance diabetes management and still have a fun time.
Read MoreIs There a Link Between Diabetes and Stress?
Are you interested in improving your diabetes management strategy by taking steps to deal with the physical and mental side effects of stress? If so, keep reading for a comprehensive overview of the link between diabetes and stress.
Read MoreWhat Is a Closed-Loop System?
Learn all about closed-loop diabetes management solutions, combining the use of a CGM and insulin pump, in this guide from US MED.
Read MoreTraveling with Diabetes: Tips for a Smooth Journey and Blood Sugar Control
Planning a trip is stressful, but managing your diabetes makes it even more challenging. US MED has all the tips you need, so you can get into vacation mode.
Read MoreGoing Back to School with Diabetes
Back-to-school season can be stressful for any parent, and there’s even more to worry about if your child has diabetes. This comprehensive guide from US MED can help make sure your prepared.
Read MoreWhat is Diabetic Neuropathy?
Find out more about Diabetic Neuropathy, including the causes, symptoms, and ways to avoid and treat this well-known diabetes complication.
Read MoreShoes, Diabetes, and Foot Health
Foot problems are common in people with diabetes, and wearing the right shoes is a great way to keep your feet safe. Learn more with US MED.
Read More10 Natural Ways to Combat Diabetes
With diabetes cases increasing in America, it’s more important than ever to take action. If you need to know how to fight diabetes naturally, these ten tips from US MED can help.
Read MoreMushrooms and Diabetes: How Can Mushrooms Help with Blood Sugar Levels?
Learn more with US MED’s guide to adding mushrooms to your diabetes diet and discover how this food can help keep your blood sugar in check.
Read MoreTips for People Newly Diagnosed with Diabetes
When you have newly diagnosed diabetes, knowing your next steps is crucial. Here are US MED’s tips for living with diabetes.
Read MoreDiabetes Support Groups: Why Are They Important?
If you’re curious about diabetes support groups but don’t know how to get started, US MED can help. Here, you’ll find our comprehensive overview.
Read MoreStaying Active with Diabetes: How Yoga for Diabetes Can Help
Following a yoga regimen could help you deal with the stress related to diabetes management. If you have type 2/type 1 diabetes and yoga sounds like something you might enjoy, keep reading for the information you need on starting a yoga routine.
Read MoreHow Does Diabetes Affect Sleep?
Are you wondering “how does diabetes affect your sleep?”. This is US MED’s overview of how sleep and diabetes type 2/type 1 intersect.
Read MoreBeing a Parent with Diabetes
When you know how to deal with diabetes, you’ll find it easier than ever to live with diabetes and raise your kids along the way. Here, you’ll find US MED’s advice for parents with diabetes.
Read MoreHow to Handle an Insulin Overdose
If you’re asking yourself “can you overdose on insulin?,” you should know this is a real possibility. Here’s the US MED guide to handling an insulin overdose.
Read MorePre-existing Diabetes and Pregnancy
Have you been looking for information on pregnancy and diabetes? If so, there’s a good chance you’re already familiar with gestational diabetes—that is, diabetes initially diagnosed mid-pregnancy. However, that doesn’t mean there’s no connection between other forms of diabetes and pregnancy. As recently as the mid-20th century, women who had type 1 diabetes were discouraged…
Read MoreDexcom G7 Release Date, Features & Cost Insights
Are you interested in learning more about the Dexcom G7 and what distinguishes it from other CGMs available today? If so, you’re in luck. Take a look at our complete overview of this exciting new product!
Read MoreKnow Your Diabetes ABCs | US MED
Learning essential diabetes management steps can make managing this disease far simpler. Learn the ABCs of diabetes with US MED.
Read MoreDoes Diabetes Cause High Blood Pressure?: Understanding Between High Blood Pressure and Diabetes
If you’re wondering, “can diabetes cause high blood pressure?” or “how can I control high blood pressure with diabetes?,” read on for all the answers you need.
Read MoreDiabetes Sweating Connection: Why Does Diabetes Make You Sweat?
Diabetes may cause you to sweat more than usual. Learn more on how diabetes and sweating are connected in the article below.
Read MoreGestational Diabetes : What Should You Eat When You’re on a Healthy Meal Plan?
Type 1 and type 2 diabetes may be the most well-known forms of diabetes, but they aren’t the only diabetes types you should be aware of. During pregnancy, you may experience a condition known as “gestational diabetes.”
Read MorePostprandial Blood Sugar: How Long After Eating Does it Take for Blood Sugar to Return to Normal?
Keeping your postprandial blood sugar under control is an essential part of living with diabetes. Here, you’ll find US MED’s in-depth explanation of postprandial blood sugar, along with tips on how to control it.
Read MoreA1C Overview: What is A1C? | US MED
One reliable method of diagnosing diabetes is the hemoglobin A1C test. If you’re asking yourself, “What is A1C testing, anyway?” Learn more with US MED.
Read MoreDiabetes Symptoms: What You Need to Know
Diabetes management isn’t always an easy task, but you’ll need to work hard at it. Learn about diabetes symptoms and management with US MED.
Read MoreDiabetes Rash: Appearance & Prevention
Diabetes can lead to complications in other areas, one of these being your skin. Learn more about what skin complications to be on the lookout for.
Read MoreHypoglycemia Symptoms, Causes and Treatments for Diabetics
Hypoglycemia is the term that is used for low blood sugar. Learn more about how people with diabetes can treat hypoglycemia.
Read MoreDiabetic Foot Pain and Soreness Causes, Symptoms, and Treatment
It’s important to know how diabetes and foot care are interlinked. Learn how to help prevent foot problems that can come with diabetes
Read MoreHow to Choose a Glucose Meter
Need to buy a new blood glucose meter? It’s essential to make sure you’re getting a glucometer that’s a good fit for your needs. Read on for frequently asked questions, simple instructions, and a brand analysis.
Read MoreBuilding a Diabetes Care Plan
There’s a lot that goes into managing diabetes, including everyday personal care, lab tests, and going to the doctor. Use our template to stay on track to manage your diabetes.
Read MoreNewsletter Sign Up
Get the latest articles, news and special offers delivered right to your inbox!
*By clicking the button above, I agree to signing up to US MED's newsletter emails and consent to receiving emails from US MED.